[ad_1]
During the last 12 months, generative AI has captivated the general public creativeness.
Many people have grow to be newly acquainted with the idea of an approaching Singularity coined by John von Neumann or Nick Bostrom’s Paper Clip thought experiment. Fortuitously, Microsoft’s workplace assistant, Clippy, has but to dutifully remodel our planet right into a heaping pile of paper clips. Nor has generative AI managed to enhance itself to a degree of surpassing human intelligence.
Apocalyptic predictions apart, generative AI does maintain the potential to trigger hurt, and these kinds of hazard fall into completely different classes. Nicely-intentioned individuals can create processes that unintentionally hurt people by failing to be clear, invading privateness or introducing implicit bias.
In a earlier article, we mentioned how generative AI within the unsuitable palms can be utilized to create supporting medical documentation for companies that by no means occurred. This will occur in medical notes, medical imaging, beneficiary verification of service letters and extra.
The excellent news is that none of those capabilities represents solely new behaviors unseen by well being care payers. Reasonably, dangerous actors can make the most of the strengths of generative AI to extend the effectivity and class of beforehand identified schemes. In different phrases, this new know-how can speed up fraud, permitting for elevated volumes of fraudulent claims submissions with fewer human sources. Well being care payers might want to reply in type.
Particular investigation items (SIU) and fee integrity (PI) professionals are essential in countering these challenges. SIU investigates and uncovers fraudulent claims, whereas PI ensures fee accuracy and compliance.
As a substitute of reinventing the wheel, utilizing generative AI can improve the effectivity of SIU and PI groups. Listed below are three examples of how these groups can use generative AI to combat again.
1. What when you had a digital assistant for claims?
One of many unstated “joys” of well being care fraud combating is the iterative dance of requesting and utilizing claims knowledge. A well-recognized state of affairs for a lot of goes like this: An investigator requests claims knowledge for a supplier from an analyst. The analyst asks questions concerning the parameters of the info pull. The investigator offers a slim set of process codes, analysis codes, timeframes, and so on. The analyst pulls the claims, and upon the investigator’s evaluate, a brand new perception requires the info to be pulled once more however with yet one more column. Rinse and repeat advert infinitum.
Nicely-intentioned individuals can create processes that unintentionally hurt people by failing to be clear, invading privateness or introducing implicit bias.
Think about having a digital assistant plugged into the claims knowledge, permitting non-technical customers to tug their knowledge. An investigator may kind in plain English, “Pull claims knowledge for Dr. Greenthumb with these procedures and diagnoses between these dates of service.” The digital assistant would even alert the person of a number of supplier identifiers and verify definitions of procedures to ask, “Would you want to incorporate all of those codes?”. Just a few rounds of this may increasingly take minutes moderately than days or even weeks of knowledge exchanges between a number of individuals.
A non-technical person may additionally run a elementary descriptive evaluation of returned claims. One may ask for probably the most prevalent mixture of diagnoses assigned by the supplier anytime two particular process codes have been billed on the identical service date. Or the person can ask for the typical variety of days between dates of service if the frequency of visits is a priority. Extraordinarily complicated parameters and evaluation would nonetheless require a technical knowledgeable, however many duties could possibly be dealt with with out one.
2. Utilizing generative AI for artificial knowledge technology
To place it mildly, coaching well being care fraud fashions is complicated. Amongst many different causes, a significant roadblock is that when you have 1000’s or tens of millions of non-fraud claims, you might solely have just a few examples of fraudulent claims in your algorithms to study from. That is identified within the machine studying group as the category imbalance drawback. One method to try to get round that is to create artificial knowledge.
Sadly, creating artificial medical knowledge is arguably much more tough than constructing the fashions that will use it. A number of components contribute to this complexity, primarily the intricacy of medical knowledge. Numerous sampling methods exist to beat this, together with lowering non-fraud examples (under-sampling), duplicating present fraud examples (oversampling), and creating new fraud examples much like present ones (artificial knowledge technology). The diagram under places this into perspective.
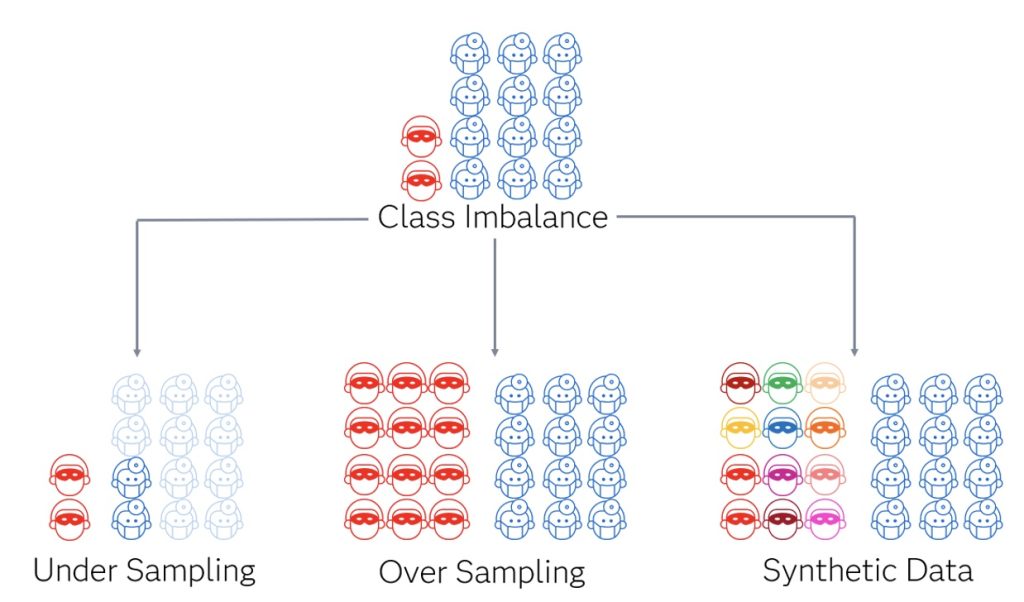
Generative AI excels within the realm of artificial knowledge technology and stands out as a result of moderately than performing duties like classifying and predicting, its output generates extra knowledge. That’s the reason it could possibly create textual content strings, photos, audio, and so on. The potential of generative AI lies in its capability to search out nuanced patterns and generate extra knowledge to look much like these fraud examples. It’s hoped that new methods will surpass earlier strategies for artificial knowledge technology for the category imbalance drawback.
3. What a few case administration assistant?
Analyzing conduct patterns in knowledge and finishing up investigations is just one piece of the fraud-fighting puzzle. Case administration is one other essential factor. It includes documenting investigative actions and process assignments, drafting communications, monitoring ROI and creating further intel by linking widespread actors and behaviors throughout a number of investigations. Most of those actions are repeatable and maintain the potential for partial automation.
Medical fraud investigations are available numerous kinds, every with distinctive nuances and necessities. The questions on nerve conduction research administration will vastly differ from questions on sturdy medical tools. A digital assistant educated for investigations can suggest questions for particular eventualities. Much like integrating a digital assistant or chatbot with claims knowledge, incorporating one right into a case administration system might be priceless to help investigators and investigative managers of their day-to-day duties. When an investigator initiates a case, step one usually includes reviewing notes and figuring out case standing. A digital case administration assistant can swiftly compile a case abstract or reply a particular query concerning the case. Additionally, it may suggest the following steps primarily based on the supplied data.
Moreover, this assistant may mine investigative case notes for extra intel. In most case administration methods, there are kinds to enter demographic identifiers about topics of curiosity, together with names, addresses, telephone numbers, license data, and so on. There may be the chance that an investigator calls a telephone quantity to succeed in a supplier. Nonetheless, this quantity is just entered into the investigative narrative moderately than a type, which means it might not be used as structured knowledge to tell analytics. An assistant may pull that quantity from the word and add it as usable structured knowledge.
The accelerating position of generative AI in fraud prevention
It shouldn’t shock anybody that generative AI is rapidly changing into a potent software. There are quite a few methods present generative AI capabilities will help payers beat the rising tide of fraud; just some are described above.
Over time, we will depend on introducing extra generative AI within the fraud area. Expertise will proceed to reinforce the power to commit fraud and combat it. Payers might want to proceed to evolve methods for detection and enhance the effectivity of conducting investigations. Now could be the time to make use of generative AI within the combat towards fraud.
Discover extra matters associated to Worldwide Fraud Consciousness Week
Jason DiNovi and Tom Wriggins contributed to this text

With over 30 years of well being care expertise, Tom Wriggins brings practitioner-level experience to his position as a Senior Supervisor with SAS. Wriggins combines in depth medical expertise with knowledge and analytics information to assist authorities and industrial well being care entities crack down on fraud and improper funds. He has led multidisciplinary groups which have delivered massive and sophisticated knowledge options for presidency well being businesses, and has created fraud and abuse investigative coaching packages.
[ad_2]
Source link



